Fractures of the Thoracic and Lumbar Spine
Cause
Fractures of the thoracic and lumbar spine may result from high-energy trauma, such as a:
- Car or motorcycle collision
- Fall from a significant height
- Sports accident
- Violent act, such as a gunshot wound
Many times, these patients have additional serious injuries that require rapid treatment. The spinal cord and/or nerves may also be injured, depending on the severity of the fracture.
Spinal fractures may also be caused by bone insufficiency. For example, people with osteoporosis, tumors, or other underlying conditions that weaken the bone can fracture a vertebra even during lower-impact events — such as reaching or twisting or falling from a standing height. These fractures may develop unnoticed over a period of time, with no symptoms or discomfort until a bone breaks.
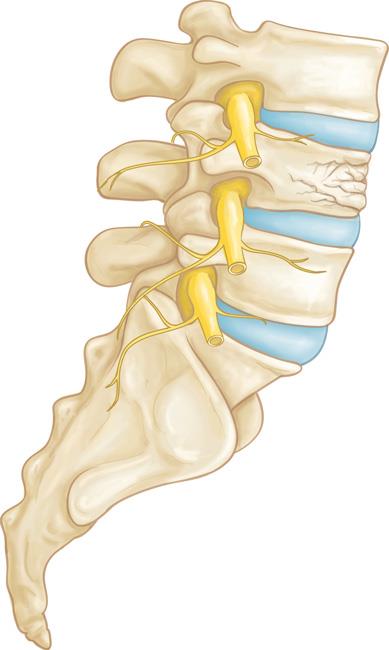
Description
There are different types of spinal fractures. Doctors classify fractures of the thoracic and lumbar spine based upon the specific pattern of the fracture and whether there is a spinal cord injury. Classifying the fracture pattern will help your doctor determine the proper treatment.
The three major types of spine fracture patterns are:
- Flexion
- Extension
- Rotation
Flexion Fracture Pattern
Compression fracture. While the front (anterior) of the vertebra breaks and loses height, the back (posterior) part of it does not. This type of fracture is usually stable (the bones have not moved out of place) and is rarely associated with neurologic problems. Compression fractures commonly occur in patients with osteoporosis.
Axial burst fracture. In this type of fracture, the vertebra loses height on both the front and back sides. It is often caused by landing on the feet after falling from a significant height. An axial burst fracture can sometimes result in nerve compression. Some fractures are stable, while others are significantly unstable (the bones have moved out of place).
Extension Fracture Pattern
Flexion/distraction (Chance) fracture. The vertebra is literally pulled apart (distraction). This type of fracture can occur in a head-on car collision when the upper body is thrown forward while the pelvis is stabilized by a lap seat belt. This is typically an unstable fracture.
Rotation Fracture Pattern
Transverse process fracture. This uncommon fracture results from rotation or extreme sideways (lateral) bending. It does not usually affect stability.
Fracture-dislocation. This is an unstable injury involving bone and/or soft tissue in which a vertebra moves off an adjacent vertebra (displacement). These injuries frequently cause serious spinal cord compression.
Symptoms
A fracture of the thoracic or lumbar spine causes moderate to severe back pain that is worsened with movement.
If the spinal cord or nerves are involved, the patient may experience bowel/bladder dysfunction along with numbness, tingling, or weakness in the limbs.
If the fracture is caused by high-energy trauma, the patient may also have a brain injury and lose consciousness, or “black out.” There may also be other injuries—called distracting injuries—that cause pain that overwhelms the back pain. In these cases, it has to be assumed that the patient has a fracture of the spine, especially after a high-energy event such as a motor vehicle crash.
Doctor Examination
Emergency Stabilization
Patients with fractures of the thoracic and lumbar spine that have been caused by trauma need emergency treatment. It may be difficult to assess the extent of their injuries on first evaluation.
At the accident scene, EMS rescue workers will first check the patient’s vital signs, including consciousness, ability to breathe, and heart rate. After the vital signs are stabilized, rescue workers will assess obvious bleeding and limb-deforming injuries.
Before moving the patient, the EMS team must immobilize the individual in a cervical (neck) collar and backboard. The trauma team will perform a complete and thorough evaluation in the hospital emergency room.
Physical Examination
The emergency room doctor will conduct a thorough evaluation, beginning with a head-to-toe physical examination of the patient. This will include an inspection of the head, chest, abdomen, pelvis, limbs, and spine.
The doctor will evaluate the patient’s neurological status. This includes testing his or her ability to move, feel, and sense the position of all the limbs. The patient’s reflexes will also be tested to help determine whether there has been an injury to the spinal cord or individual nerves.
The doctor may also check the tone of the anal muscles and determine whether the patient is able to empty his or her bladder without assistance. Problems with bowel and bladder function may indicate a more serious spinal cord injury.
Tests
Imaging tests. After the physical examination, a radiologic evaluation is required. Depending on the extent of the injuries, this may include X-rays, computerized tomography (CT) scans, and magnetic resonance imaging (MRI) scans of multiple areas, including the thoracic and lumbar spine.
Treatment
Treatment for a fracture of the thoracic or lumbar spine will depend on:
- Other injuries and their treatment
- The particular fracture pattern
- Whether there is neurological injury
Once the trauma team has stabilized all other life-threatening injuries, the doctor will evaluate the spinal fracture pattern and decide whether spine surgery is needed.
Flexion Fracture Pattern
Nonsurgical treatment. Most flexion injuries–including stable burst fractures and osteoporotic compression fractures—can be treated with bracing for 6 to 12 weeks. By gradually increasing physical activity and doing rehabilitation exercises, most patients avoid post-injury problems.
Surgical treatment. Surgery is typically required for unstable burst fractures that have:
- Significant comminution (multiple bone fragments)
- Severe loss of vertebral body height
- Excessive forward bending or angulation at the injury site
- Significant nerve injury due to parts of the vertebral body or disk pinching the spinal cord
- Ligament damage that makes the spine unstable
These fractures should be treated surgically with decompression of the spinal canal (if there is nerve damage) and stabilization of the fracture. The procedure to decompress the spine is called a laminectomy. In a laminectomy, the doctor removes the bony arch that forms the backside of the spinal canal (lamina), along with any bone or other structures that are pressing on the spinal cord. Laminectomy relieves pressure on the spinal cord by providing extra space for it to drift backward.
To perform the laminectomy, your doctor will access your spine with an incision either on your side or on your back. Both approaches allow for safe removal of the structures compressing the spinal cord, while preventing further injury.
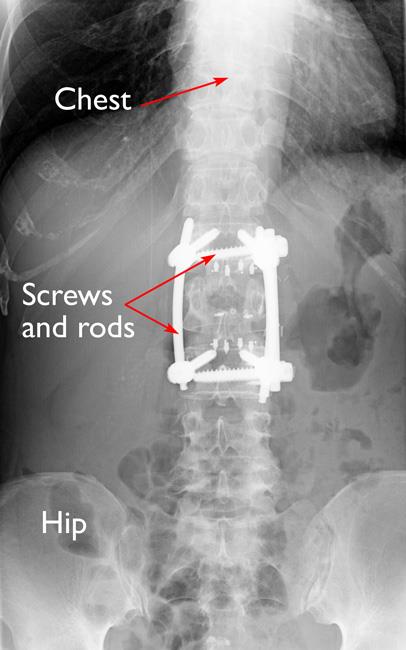
After the laminectomy, your doctor will stabilize the fracture by reconstructing the damaged bone or placing screws above and below the fracture.
Extension Fracture Pattern
Treatment for extension injuries will depend on:
- Where the spine fails
- Whether the bones can be fit together again (reduction) using a brace or cast
Nonsurgical treatment. Extension fractures that occur only through the vertebral body can typically be treated without surgery. These fractures should be observed closely while the patient wears a brace or cast for 12 weeks.
Surgical treatment. Surgery is usually necessary if there is an injury to the posterior (back) ligaments of the spine. In addition, if the fracture falls through the disks of the spine, surgery should be performed to stabilize the fracture.
Rotation Fracture Pattern
Nonsurgical treatment. Transverse process fractures are predominantly treated with a gradual increase in motion, with or without bracing, based on comfort level.
Surgical treatment. Fracture-dislocations of the thoracic and lumbar spine are caused by very high-energy trauma. They can be extremely unstable injuries that often result in serious spinal cord or nerve damage. These injuries require stabilization through surgery. The ideal timing of surgery can often be complicated. Surgery is sometimes delayed because of other serious, life-threatening injuries.
Surgical Procedure
The ultimate goals of surgery are to:
- Achieve adequate reduction (return the bones into their proper position)
- Stabilize the fracture
- Relieve pressure on the spinal cord and nerves
- Allow for early movement
Depending on the fracture pattern, the doctor may perform the procedure through either an anterior (front), lateral (side), or posterior (back) approach—or a combination of all three.
There are many types of specialized instruments used in spine surgery. These include metal screws, rods, and cages used to stabilize the spine.
Complications
Complications associated with fractures of the thoracic and lumbar spine include:
- Blood clots in the pelvis and legs—these may develop during long periods of bed rest or immobility
- Pulmonary embolism—a blood clot that breaks free and travels to the lungs
- Pneumonia
- Pressure sores
There are also specific complications associated with spinal surgery. These include:
- Bleeding
- Infection
- Spinal fluid leaks
- Instrument failure
- Nonunion
- Wound complications
Your doctor will talk with you about these risks and take specific measures to avoid potential complications. These measures may include:
- Early treatment
- Mechanical methods (such as lower leg compression stockings) and medications to protect against blood clots
- Proper surgical technique
- Postoperative programs
Outcomes
Regardless of whether treatment is surgical or nonsurgical, there will be a period of rehabilitation after a fracture has healed.
The goals of rehabilitation include:
- Reducing pain
- Restoring mobility
- Returning the patient as closely as possible to his or her preinjury state
Your doctor may recommend both inpatient and outpatient physical therapy to help you achieve these goals.
If your fracture was caused by osteoporosis, you are at an increased risk for additional fractures. Your doctor will recommend treatments to address bone density loss during your treatment and recovery.
In some cases, there may be issues that delay or complicate rehabilitation and recovery. These issues include inadequate reduction of the fracture, neurologic injury (paralysis), and progressive deformity of the spine.